I always find it interesting how bewildered most people are – including physicians and healthcare administrators – when asked about the opioid epidemic. Most point to societal factors and unstable family structure as primary causes and there is ample evidence to support this view. However, a significant factor – and one that is not often discussed – is the role of physicians, their administrators and medical practice guidelines prevalent in the 1990’s.
I am not going to try and simplify things. Honestly, there are many causes of the opioid epidemic. However, one often overlooked fact is that changes in the practice of medicine that took place in the 1990’s – changes that really were well-meaning – actually contributed to opioid addiction. Moreover, these changes were tied to reimbursement – particularly for hospitals – so physicians and hospitals had to “play the game” or risk losing funding and employment.
 Back in the 1980’s when I was training to become a doctor, we probably under-treated pain. Pain medicine was used to “take the edge off” but neither patient nor doctor expected the medication to remove pain entirely. As training physicians in an urban setting, we were aware of the risks of addiction and definitely subscribed to the “less is more” philosophy of pain management.
Back in the 1980’s when I was training to become a doctor, we probably under-treated pain. Pain medicine was used to “take the edge off” but neither patient nor doctor expected the medication to remove pain entirely. As training physicians in an urban setting, we were aware of the risks of addiction and definitely subscribed to the “less is more” philosophy of pain management.
Things changed a lot during the 1990’s. Probably the most significant change was the adoption of a well-meaning but soon to be abused phrase – put forward by the American Pain Society in 1996 – PAIN IS THE 5th VITAL SIGN. In other words, in addition to Pulse, Blood Pressure, Temperature and Respiratory Rate every patient had to be assessed for pain. In theory, this wasn’t a bad idea as it prevented under-treatment of pain. However, as is often the case, the pendulum swings too far in the opposing direction. All of a sudden, this slogan became more of a mantra.
This mantra echoed in the halls of Congress and soon a patient’s perception of pain management became tied to Medicare and Medicaid reimbursement. Hospitals were told that to receive maximum payment for their services, patients had to complete surveys indicating whether their pain was managed appropriately in the hospital. Poor scores on this metric would lead to poor reimbursement rates. This would “trickle down” to lower salaries, less resources, etc.
 What happened as a result? Hospital administrators pushed physicians (particularly those working the Emergency Department) to prescribe more pain medication. As one hospital administrator (who will go unnamed) once said to me “Over-treat don’t Under-treat Pain. A patient who is overmedicated and/or asleep doesn’t complain.”
What happened as a result? Hospital administrators pushed physicians (particularly those working the Emergency Department) to prescribe more pain medication. As one hospital administrator (who will go unnamed) once said to me “Over-treat don’t Under-treat Pain. A patient who is overmedicated and/or asleep doesn’t complain.”
Sadly, as physicians, we didn’t stand up to this clearly misguided rhetoric. Medical training is similar to military training in many respects. You don’t question your superiors, especially hospital CEO’s. You just do as you are told. And so we did. ER docs started prescribing Percocet like water, Dilaudid became the new Tylenol, etc. Patients completed their surveys and went home with prescriptions for Percocet and other opioids. The resourceful ones even “threatened” ER docs and staff with a poor review if they didn’t get the prescriptions they wanted.
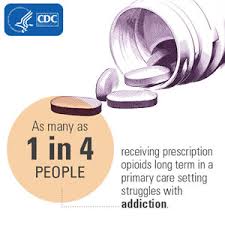
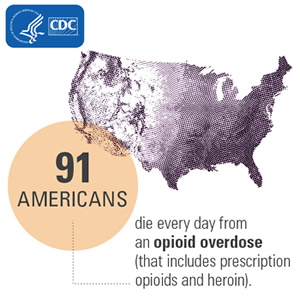
… And so a new generation of addict was born. This was not the heroin addict of the 1960’s – injecting bags of dope in bad neighborhoods. This was blue collar and white collar men and women with large mortgages and little savings running on the hamster wheel of economic prosperity who were simply overwhelmed. They wanted a magic pill to make their problems go away – at least for awhile. And they got it – in the form of semi-synthetic opioids.
The question is not how we got here. It is how do we get away from here.
