The following is a rather long article because I didn’t want to try and oversimplify the problem of addiction treatment brokers. This isn’t a subject that can be discussed in a paragraph or explored in a 2 minute sound bite. This issue is complex and I want to avoid the “throw the baby out with the bath water” approach that many, including Google have proposed and implemented because that approach, as expedient as it may seem, may lead to an even more tragic outcome for those in need of addiction treatment.

As an addiction treatment professional it is gratifying to see that the disease of addiction is finally receiving the attention it deserves – from the media, from the public and most importantly, from politicians who are empowered to fund treatment and prevention programs. Most of these programs are of high quality, staffed by competent and compassionate counselors and medical personnel who work in this field not for financial remuneration but because they want to make a difference. In fact, as a primary care physician who chose the sub-specialty of Addiction Medicine as opposed to other more lucrative choices, I knew I was trading better pay for the privilege of helping those in need put their lives back together.
For several years I have worked with addicted patients and have advocated for the field of Addiction Medicine, largely through my work with ASAM (the American Society of Addiction Medicine) and NYSAM (the New York Society of Addiction Medicine). I can’t tell you how many of my letters and phone calls to politicians and policy makers went unanswered from 2000 through 2010 – as I tried to sound the warning about the opioid epidemic as loudly as possible. Then I watched helplessly as well-meaning politicians with little understanding of addiction hurriedly passed laws and enforced regulations that although well-meaning, drove patients from prescription opioids to heroin increasing rather than decreasing the rate of overdose. These consequences may have been a surprise to lawmakers but they certainly were not a surprise to my Addiction Medicine colleagues and I.
Now I fear that a new development and the proposed response to it may once again hurt more people than it helps. Since the field of Addiction Medicine is finally getting the respect and funding it deserves, we have run into a new problem: the emergence of opportunists who see a way to make money by marketing themselves as a gateway to treatment. What I am referencing here are treatment “brokers” and the way they have used Google search and Adwords to create a business model that I believe is immoral and unfair. By dominating Google search (through a combination of web design savvy and their willingness to pay enormous sums for addiction-related keyword bids), they insert themselves as middlemen between addicts and treatment centers, making it difficult to find actual treatment centers or addiction medicine professionals without going through them first. Moreover, their presence drives up the price of advertising through Google Adwords to the point where actual addiction specialists and treatment programs can no longer afford to advertise treatment services as such programs usually operate with small budgets with little or no profit margin.
In other words, when it comes to advertising for addiction treatment the playing field is most certainly not level. Treatment brokers have little or no overhead as they don’t actually provide treatment. They don’t need a building or counseling staff. They simply build a flashy website and hire an operator who answers the phone and refers patients to the treatment programs that can afford to pay huge sums to brokers for such referrals. Those treatment programs are not recommended by the broker because they are good and most appropriate for a given patient, but because such treatment programs pay dearly for such referrals. Of course, a program that must spend large sums for such referrals cannot also afford to hire the best professionals to provide evidence-based addiction treatment so it faces a choice: either it can raise the cost of treatment to the point where most people can’t afford it (it is not unheard of for a month-long treatment to exceed $30,000) or hire cheaper staff who are less competent and qualified.
Although I imagine that Google was unaware of this practice until recently, their bid-based advertising model has made them complicit in this scam. After the following New York Times article exposed this business practice and Google’s active although unwitting complicity – https://www.nytimes.com/2017/09/14/business/google-addiction-treatment-ads.html – Google bowed to pressure and reacted by pulling virtually all addiction treatment ads for their site. However, this un-nuanced, all be it well-meaning knee-jerk response – could actually have more tragic repercussions for addicts than making no changes at all as it “erases” legitimate treatment programs as well as these brokers. In other words, as Google, for all practical purposes, has a monopoly on search, removing all ads for treatment professionals and programs will likely result in the addict or his/her family believing that no quality addiction treatment is available locally, when, in fact, that is not actually the case.
What Google is attempting to do here is to wash its hands of the problem so it can focus on less controversial industries. I understand the company’s reasoning but In my view, that approach is not acceptable. The bidding war for keywords (which is a direct result of the Google Adwords model) created this problem. As a socially responsible company (which, I believe, it tries to be) Google itself must directly address this issue. By taking a small percentage of the legitimate profits Google can generate from the advertising of qualified treatment professionals and treatment programs, Google can help to “police” itself and the addiction treatment industry, providing links to legitimate treatment providers while excluding the treatment brokers that have tarnished its reputation.
The issue at hand is how to most efficiently and fairly vet treatment providers so the legitimate ones are given a Google “good housekeeping” seal of approval, allowing them to advertise and publicize their services through the search engine. I realize there are no easy solutions here – but if treatment professionals and the advertising professionals at Google are given the chance to work together, I am sure we could create an effective and equitable system where providers are vetted before their ads go “live”.
In terms of physicians, this vetting process is relatively easy because much of the work has already been done. First, physicians are required to file a lot of paperwork to maintain licensure to practice medicine. In addition, in my view, anyone who calls himself/herself an addiction specialist should be Board Certified by the American Board of Addiction Medicine or the American Society of Addiction Psychiatry, two credible organizations that require physicians to stay current in this rapidly developing field. As medication assisted treatment for opiate dependence is now the “standard of care”, any addiction specialist should also have the SAMSHA waiver to provide buprenorphine. Lastly, a treatment facility wishing to advertise on Google should employ an Addiction Medicine physician as its medical director and Medication Assisted Treatment should be an option for patients who request it.
On the counseling side, treatment programs should be required to hire qualified counselors who are licensed by the state in which they practice. In New York, for example, counselors may have a social work license, a psychology license or be Certified Alcohol and Substance Abuse Counselors. Of course, every state has different licensing requirements so criteria will have to be tweaked depending on program and provider location.
My point here is that this is not rocket science. With a well-thought strategy, Google can help the addiction treatment industry to police itself, removing the few bad actors who do not adhere to high treatment standards. This is not to say that we need Google to be “Big Brother”. There are certainly different legitimate evidence-based approaches to care and there is no need for every provider to practice addiction treatment in exactly the same manner. From diversity comes innovation and I understand that. However, as in other fields of medicine, I think we can agree on some broad guidelines. Medication Assisted Treatment is good. Putting leaches on someone to cure his/her addiction is not. Agreed?
In my view, we all need to step out of our bubbles for a minute. Treatment providers and technology giants like Google must work together to guide those suffering from the deadly disease of addiction to safe and reputable care. Opportunists hijacked technology to create the problem. Trusted treatment providers and software engineers working together can solve it.









 Back in the 1980’s when I was training to become a doctor, we probably under-treated pain. Pain medicine was used to “take the edge off” but neither patient nor doctor expected the medication to remove pain entirely. As training physicians in an urban setting, we were aware of the risks of addiction and definitely subscribed to the “less is more” philosophy of pain management.
Back in the 1980’s when I was training to become a doctor, we probably under-treated pain. Pain medicine was used to “take the edge off” but neither patient nor doctor expected the medication to remove pain entirely. As training physicians in an urban setting, we were aware of the risks of addiction and definitely subscribed to the “less is more” philosophy of pain management.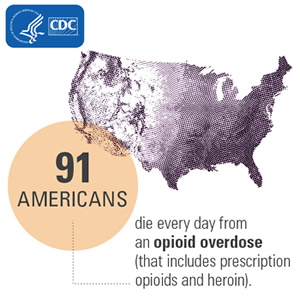 What happened as a result? Hospital administrators pushed physicians (particularly those working the Emergency Department) to prescribe more pain medication. As one hospital administrator (who will go unnamed) once said to me “Over-treat don’t Under-treat Pain. A patient who is overmedicated and/or asleep doesn’t complain.”
What happened as a result? Hospital administrators pushed physicians (particularly those working the Emergency Department) to prescribe more pain medication. As one hospital administrator (who will go unnamed) once said to me “Over-treat don’t Under-treat Pain. A patient who is overmedicated and/or asleep doesn’t complain.”